The Pelvimetry Plot Twist
Why Your 1950s Measurements Might Be All Wrong
Here's a question that might make you pause: When was the last time you questioned whether the pelvic measurements we've been using since your grandmother's era are actually... accurate?
Buckle up, because we're about to dive into one of obstetrics' best-kept secrets – and it's more fascinating than you'd think.
The Great Pelvimetry Time Warp
It's 2025, you're using AI to read mammograms and robots to assist surgeries, but when it comes to pelvimetry, you're still relying on standards set in the 1950s. Sounds a bit like using a flip phone to run your practice, doesn't it?
Recent research from France has dropped a bombshell that's got the obstetric world buzzing. A comprehensive study analysing 551 CT pelvimetries revealed something eye-opening: our current "normal" values might be seriously outdated. The researchers found that modern women's pelvic dimensions don't quite match those decades-old textbook numbers we've been faithfully following.
Here's the kicker – the median obstetric transverse diameter they found was 12.41 cm, with the 3rd percentile at 11 cm. These numbers; they represent real outcomes that could reshape how we approach delivery planning.
The Tech Tango: CT vs. MRI vs. Good Old Clinical Judgment
Now, let's talk tech. The imaging world has been having its own quiet revolution while we weren't looking. Remember when X-ray pelvimetry was the gold standard? Those days are fading faster than your energy after a 24-hour call.
CT pelvimetry has stepped up its game dramatically. Modern low-dose techniques have slashed radiation exposure from a whopping 50 mGy down to just 2.5 mGy – that's a 95% reduction! Meanwhile, MRI pelvimetry is making waves with its radiation-free approach, showing remarkable agreement with CT measurements.
But here's where it gets interesting: Despite all this technological wizardry, studies consistently show that pelvimetry's predictive power for labor outcomes remains... well, let's call it "humble." One study found accuracy rates hovering between 50-74% for predicting labor outcomes. Not exactly the crystal ball we were hoping for, right?
The Real-World Reality Check
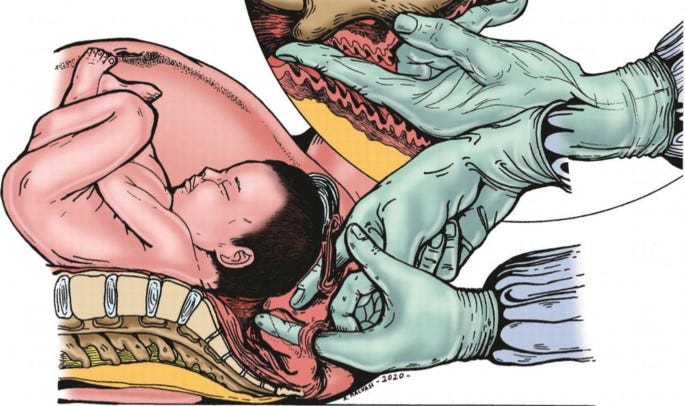
Here's what's really happening in delivery rooms: The research suggests that women who undergo X-ray pelvimetry are more likely to end up with cesarean sections. But is this because pelvimetry accurately predicts difficult deliveries, or because having those measurements influences our decision-making in ways we don't fully realize?
It's like having a weather app that's right half the time – useful information, but maybe not something to plan your entire vacation around.
So where does this leave us ?
First, it's time to acknowledge that pelvimetry isn't the definitive answer we once thought it was. The evidence suggests its greatest value might be in specific clinical scenarios – think breech presentations or cases where you're genuinely on the fence about delivery planning.
Second, if you're still using those 1950s reference values, it might be time for an update. The French study represents the largest modern dataset we have, and those numbers are worth incorporating into your clinical thinking.
Finally, remember that technology is a tool, not a replacement for clinical judgment. Whether you're using state-of-the-art 3D CT reconstruction or good old-fashioned clinical assessment, the art of obstetrics still lies in combining multiple data points to make the best decisions for each unique patient.
Pelvimetry is having its moment of reckoning – and honestly, it's about time.
As we embrace personalized medicine and precision healthcare, maybe it's time to give our pelvic assessments the same modern makeover.
What's your take on pelvimetry in modern practice? Hit reply and share your thoughts – I'd love to hear from you!
A quick reminder for an opportunity to up-skill
Master Endometriosis Surgery with Mayflower – CSEEMIG Batch 15
📅 _July 22nd - 25th, 2025
📍 Mayflower Women's Hospital, Ahmedabad
Mayflower’s record in endometriosis care speaks for itself – a recurrence rate of less than 2%, far below the global average of 20-40%. This consistency is no accident.
The institute opens its doors once again, offering an opportunity to witness the approach that has set this standard.
Observe Dr. Sanjay Patel, Dr Smeet Patel and the iconic Mayflower Endo Team perform live surgeries featuring advanced techniques like the Butterfly Peritonectomy and Rule of M.
Gain insight through case discussions, Q&A sessions, and shared experiences with peers.
Registration and Payment
Endometriosis Weekly Update —
How Communication Shapes Endo Care
This article explores 3 common ways people unintentionally harm endometriosis patients through words—like minimization and toxic positivity. A quick, essential read for anyone in healthcare or caregiving.