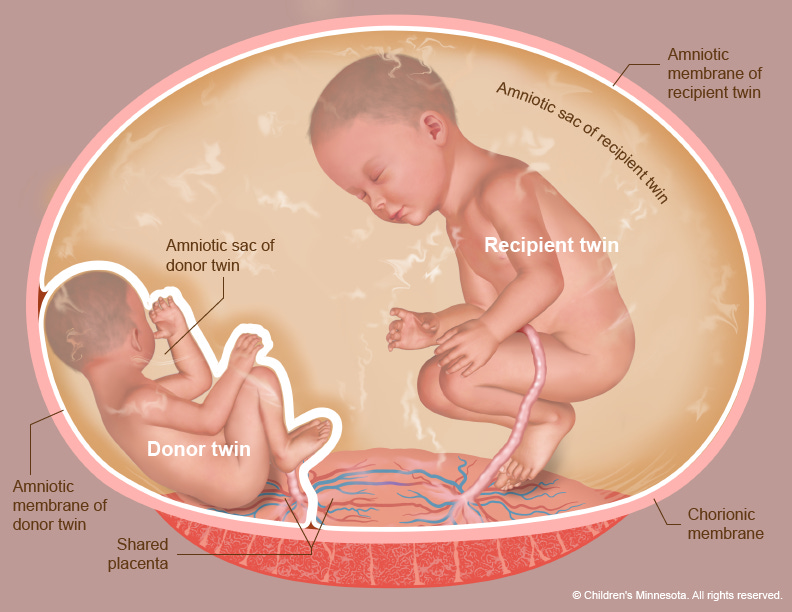
A couple came, twenty weeks into what should be the most thrilling chapter of their lives, shuffling into our fetal medicine unit clutching a thick file of ultrasound prints and devastating news: Termination may be your safest option. Their twins shared a single placenta—the monochorionic setup that, in about one pregnancy out of seven, flips into Twin-to-Twin Transfusion Syndrome (TTTS). One baby guzzles blood and nutrients; the co-twin is left running on fumes. Untreated, the odds tip toward heart failure, preterm delivery, even the loss of both babies.
They had already burned miles and money on second and third opinions. Every door seemed to lead abroad—Europe if the paperwork cooperated, the U.S. if the wallet didn’t scream first. Then someone whispered a new name into the mix: Mayflower Women’s Hospital, Ahmedabad.
Enter Dr. Mayank Chowdhury, our resident wizard of fetal medicine at Mayflower Women’s Hospital, and his long-time mentor Dr. S. Suresh on the remote console. Together they proposed a plan that sounded part sci-fi, part high-wire act: fetoscopic laser photocoagulation. In plain English, slide a 3 mm camera into the uterus, map the rogue vessels on a living placenta in real time, and weld them shut with laser light—all without disturbing two heartbeats and one very anxious mother. Globally, only a handful of teams attempt it. In western India, precisely zero had logged a success.
Surgery day was equal parts choreography and nerve.
Under regional anesthesia, Dr. Mayank eased the fetoscope through a sub-centimetre entry and—with the subtle steering you’d expect from a seasoned gamer rather than a surgeon in his fifties—navigated to the vascular tangle. Each aberrant connection flashed, fizzed, and sealed. Forty-seven minutes later the scope came out, the incision closed with a single stitch. On the monitor, twin A’s over-distended bladder had already shrunk to normal; twin B’s amniotic desert was refilling.
Post-op scans over the next 24 hours sealed the verdict:
balanced Dopplers, stable heart rates, two babies happily kicking walls. The mother is now on a tight follow-up leash—fortnightly growth scans, Dopplers, the entire fetal-cardiac jazz band. But the crisis has been averted.
Why should this make your ears perk up? Because until last week, TTTS referrals from Gujarat and much of South Asia could only head to Chennai or cross continents. That delay—plus the cost—kills access. By adding fetoscopic laser to Mayflower’s toolbox, we’ve chopped the travel time to hours, slashed the bill to a fraction, and kept families in their own language zone.
More important, we’ve planted a regional safety net: if you spot discordant fluid levels or growth in monochorionic twins between 16 and 26 weeks, you now have a local address for definitive therapy.
A few clinical postcards for your next case conference:
Ideal window: 18–22 weeks (we squeaked in at 20).
Quintero Stage II+ is your trigger to phone a fetal surgeon.
Procedure length: 45–60 minutes; maternal hospital stay, overnight.
Survival odds: over 85 % for at least one twin when treated, versus 10 % if you let TTTS run its grim course.
Dr. Mayank isn’t finished. He’s drafting shared protocols so you can screen twins early, lobbying insurers for laser-therapy coverage, and mentoring the next generation of fetal surgeons—because one centre is great, but a network saves more babies.
So, the next time your monochorionic twins start looking lopsided, remember: the lasers are now in Ahmedabad. Drop us a call, and let’s tip the odds back in favour of two healthy cries in the delivery room—no passport required.
AND if you’re looking to learn from the likes of Dr. Mayank Chowdhury, Dr. Sanjay Patel, Dr. Smeet Patel, and the star team at Mayflower Women’s Hospital — here’s your chance.
CSEEMIG Batch 15 is coming up soon!
📅 July 22–25, 2025
📍 Mayflower Women’s Hospital, Ahmedabad
With a recurrence rate of under 2% — well below the global average — Mayflower’s endometriosis care is considered a national benchmark.
In this 4-day hands-on course, you’ll:
🔹 Observe live surgeries with advanced techniques like Butterfly Peritonectomy and Rule of M
🔹 Attend focused case discussions and Q&A sessions
🔹 Learn the structured protocols behind their consistently excellent outcomes
Limited seats. Apply early.
Have you filled the Endometriosis India Survey yet?
This short, anonymous survey is an effort to gather real insights from doctors who are treating endometriosis in real-world settings — not just from those on conference panels. It covers key areas like how you diagnose the disease, your approach to treatment and surgery, post-op care, pricing, and collaboration.
The goal is to better understand how gynecologists and laparoscopic surgeons across India are currently managing endometriosis. Each response helps build a more accurate picture of what’s happening on the ground — and gives the wider community a chance to learn from shared patterns.
It only takes a few minutes, and all questions are optional. No names or data are collected unless you choose to share.
And if you’ve already submitted your response, thank you — please consider forwarding it to a colleague. The more the responses, the stronger the insights.
Thanks for reading Pollen by Mayflower! If you liked what you read and would like to read more of it, please subscribe and receive regular updates from Mayflower.
And if you think a friend would love to read this, feel free to share it with them too. We’d appreciate it :)